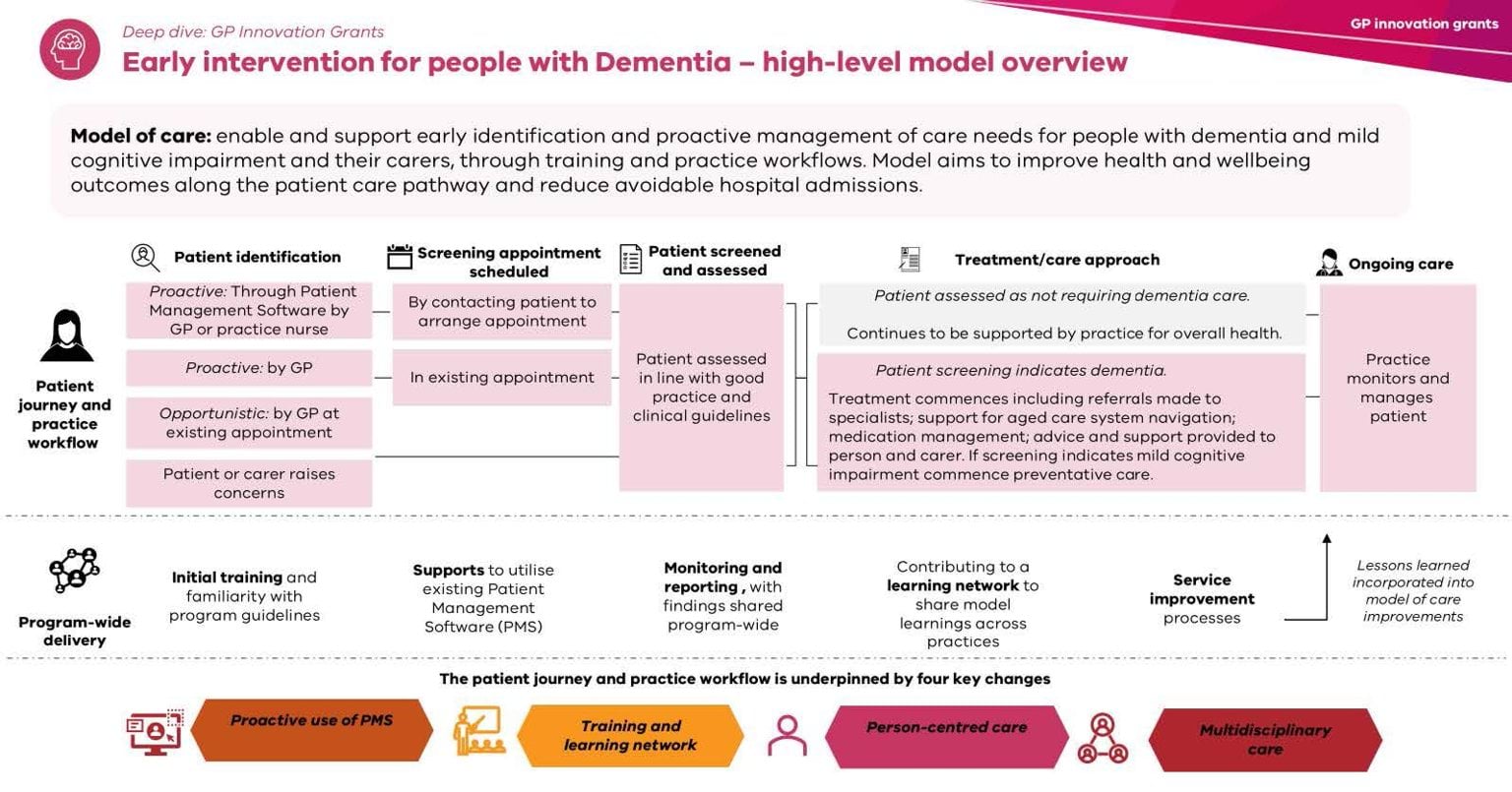
The Model of Care supports early identification and proactive management of care needs for people with dementia and mild cognitive impairment and their carers.
Key elements
The Model of Care has four key areas of focus;
- Proactive use of Patient Management System (PMS): proactive use of patient management software to fund patients at risk of dementia or cognitive impairment.
- Training and learning network: improving General Practitioner knowledge and confidence through training and participation in a learning network.
- Person-centred care: utilising the skills and expertise of general practice in dementia care through improving capacity to provide coordinated person-centred care.
- Multidisciplinary care: utilising funding to enhance multidisciplinary care, particularly practice nurses.
Proactive use of patient management software
Why it matters
High-quality routinely collected general practice data can identify a range of different risk factors including lifestyle characteristics, physical activity, social engagement, as well as diagnoses and medications.
General practices can proactively utilise their patient management software to identify patients at risk of dementia, in alignment with the outlined target cohort and risk factors.
How to implement
All participating general practices will proactively target patients by identifying the following risk factors, where possible:
- Non-modifiable risk factors including ageing (people 60+), family history of the condition and other genetic mutations or variation.
- Modifiable risk factors including tobacco use, excessive alcohol consumption, physical inactivity, obesity, high low-density lipoprotein (LDL) cholesterol, limited education, hypertension, depression, diabetes, traumatic brain injury, low social contact, exposure to air pollution, untreated vision loss, hearing loss.
- Risk factors for Aboriginal and Torres Strait Islander people also include childhood stress and trauma and low socioeconomic status.
Training and learning network
Why it matters
Research shows that participation in structured training can significantly improve primary healthcare workers’ knowledge, as well as confidence in the early identification and diagnosis of dementia patients.
A training and learning network will support improved knowledge and confidence in dementia care, identify best practices, and support the broader roll out of the Model of Care.
How to implement
All participating general practices will:
- Participate in the training and learning network,
- Ensure staff access and utilise resources and training recommended by the network.
Person-centred care
Why it matters
Person-centred care places the individual at the heart of their care, recognising their unique needs, preferences, values, and circumstances, while acknowledging that people’s experiences with dementia is unique and personal.
How to implement
All participating general practices must practice person-centred care in accordance with the NHMRC Clinical Practice Guidelines and Principles of Care for People with Dementia, by identifying, screening and responding to individual needs and preferences of the person with dementia, their family and carers.
Multidisciplinary care
Why it matters
Multidisciplinary care brings together healthcare professionals from different disciplines to collaborate and provide holistic, comprehensive, and coordinated care. This ensures the diverse needs of individuals, particularly those with complex or chronic conditions, are effectively addressed.
Practice nurses play a vital role in patient care before, during and after general practitioner care and are critical in promoting quality of care, as well as providing ongoing communication with families and carers.
How to implement
All participating general practices will utilise a team-based and collaborative approach to care, particularly between general practitioners and nurse practitioners to promote good practice dementia primary care.
Note: The Victorian Government is committed to providing a website that is accessible to the widest possible audience, regardless of technology or ability. The graphic above may not meet our minimum WCAG AA accessibility standards. If you are unable to read this content you can contact the content owners for an accessible version.
Updated